Video Transcript:
Hey everyone. Julian Corwin here, Pain and Performance Solutions, Santa Rosa, California.
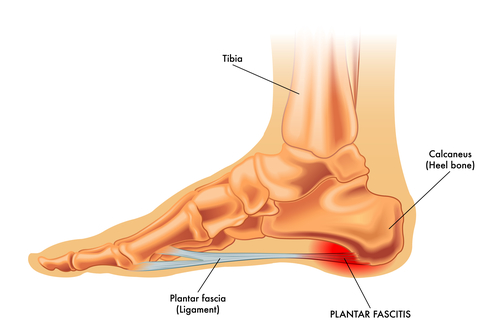
Just wanted to talk to you today about one problem that has two names, and that is plantar fasciitis and Achilles tendonitis. You might be wondering how are those in any way the same thing. Sure, you have inflammation in two different areas so there’s two different names, but they’re usually caused by the same set of problems.
The problem isn’t originating from where you have the inflammation, the itis. It’s where are the mechanics wrong that are setting your body up to inflame a certain area and try and heal it, and sets up the cyclical cycle of healing and pain and inadequate healing and sometimes it even sets up a cyclical cycle such as as we inflame an area it actually gets less mobile and the the problem just worsens itself.
Where we see interventions like a cortisone injection actually work is instances like this where the immobility from the inflammation itself is of paramount importance, but it usually doesn’t last and usually got to do something else to fix the problem.
So, what are some potential solutions? First, we want to look locally at the foot and then go global from there. Look at the posterior chain and things that could cause excess tension on the plantar fascia or the Achilles tendon. So, what I’ll have you do is we’ll take a quick look at your feet. We’re going to assess two different areas of the foot; the big toe and then the heel.
Okay. So, I’m just going to set the camera down here looking at the foot. We want to be able to extend the toe 60 degrees. And when we push the toe up let’s say you just set your foot down like so and you grab a hold of the big toe and pull it up you want to see some arching of that medial arch here. Okay. From up above, if you were to look down at your foot, you’d also want to see that when you pull this, this whole complex known as the subtalar joint kind of rotates or the talus rotates out externally. You see the arching and the movement of this bone laterally.
That will give us a good idea if whether or not your calcaneus and tailles are actually moving. If they’re not moving, then your plantar fascia is essentially like a bowstring on a bow that’s being fired with no arrow in it, i.e. all of the forces are being dumped into the attachment points into the bone and hence all the inflammation.
So, I’m just going to show you on the foot model here. So, this bone here plantar flexes when we’re loading up the plantar fascia, and it dorsiflexes when we’re unloading it. And this bone also rotates in medially and laterally when we pronate and we supinate. The big toe joint is this guy over here, and we want to make sure he has 60 degrees range of motion.
So, to quote David Weinstock, Founder of NKT and one of my teachers, “Start local, go global.” Now let’s talk about the global patterns we would want to be looking at. I’m going to take you over here to a Thomas Myers Anatomy trains poster of the posterior superficial back line, i.e. posterior chain or a.k.a posterior chain. Plantar fascia is here. Achilles tendon is here. Gastocnemius, hamstrings, sacrotuberous ligament, erector spinae muscle group. This fascia extends all the way to the forehead. You can even look at head injuries as a possible relationship with the tendonitis or fasciitis.
Anyways, want to be checking the big muscle that’s not included here, the gluteus maximus as well as the hamstrings and anything else along this line as whether or not they’re working. So, you would assess that with a technique like neuro kinetic therapy or other manual muscle testing techniques. Just do a manual muscle test on those.
You need a therapist for this. So, look up someone who does NKT in your area. Anyways that should give you some ideas about what could be causing Achilles tendonitis and plantar fasciitis, and I want to add an important caveat here. This applies to the unilateral case. That is when you only have pain on one side. If you have pain on both sides, you got to be looking in the core, at the spine, at a head injury as a possible causative mechanism for why you have Achilles tendonitis or plantar fasciitis.
So, in order of importance I would rank the mobility of the heel and the ankle as number one. The mobility of the big toe as number two, and then probably hamstrings and glutes as three and four. Probably glute as actually more likely not working than the hamstrings. Oftentimes in these cases you do need some sort of way to knock down the inflammation to boost healing. I wouldn’t recommend ice. Definitely want to be heating that, moving it, getting some increased blood flow, some sort of recovery mechanism so that the fluids that are trapped there causing inflammation, you can get them out. Voodoo floss band would be great for that. Garbage out, groceries in so you can heal that fascial band, that tendon best you can while you’re restoring the mechanics so that it doesn’t come back.
I hope that’s helpful. Shoot me a message if you have any more questions. All right, cheers.
FAQ Section: Understanding Plantar Fasciitis and Achilles Tendonitis
1. What are the primary causes of plantar fasciitis and Achilles tendonitis?
Plantar fasciitis and Achilles tendonitis typically stem from biomechanical issues and improper foot mechanics. These conditions can be aggravated by factors like overuse, improper footwear, and inadequate stretching.
2. How are plantar fasciitis and Achilles tendonitis related?
Although plantar fasciitis and Achilles tendonitis affect different areas, they often share common underlying causes. Both conditions involve inflammation due to mechanical stress and improper movement patterns in the foot and ankle.
3. What role do foot mechanics play in the development of these conditions?
Faulty foot mechanics, such as overpronation or supination, can place excessive strain on the plantar fascia and Achilles tendon, leading to inflammation and pain. Addressing these biomechanical issues is essential for preventing and managing plantar fasciitis and Achilles tendonitis.
4. How can muscle tension impact the risk of developing these conditions?
Excessive muscle tension, particularly in the calf muscles and posterior chain, can contribute to the development of plantar fasciitis and Achilles tendonitis. Tight muscles can alter foot mechanics and increase stress on the affected tissues, predisposing them to injury.
5. What are some effective treatment options for plantar fasciitis and Achilles tendonitis?
Treatment options for plantar fasciitis and Achilles tendonitis may include rest, ice, stretching exercises, orthotic devices, and physical therapy. In some cases, cortisone injections or surgery may be necessary to alleviate symptoms and restore function.
6. How does improper footwear contribute to these conditions?
Wearing shoes with inadequate support or cushioning can exacerbate plantar fasciitis and Achilles tendonitis by placing additional stress on the foot and ankle. Choosing footwear with proper arch support and shock absorption is crucial for preventing these conditions.
7. What are some preventive measures individuals can take to avoid plantar fasciitis and Achilles tendonitis?
Preventive measures include maintaining a healthy weight, wearing supportive footwear, warming up before exercise, and gradually increasing activity levels. Incorporating regular stretching and strengthening exercises can also help improve foot mechanics and reduce the risk of injury.
8. How can muscle imbalances contribute to the development of these conditions?
Muscle imbalances, such as weakness in the calf muscles or tightness in the posterior chain, can disrupt normal foot mechanics and increase the risk of plantar fasciitis and Achilles tendonitis. Addressing these imbalances through targeted exercises and stretches is essential for preventing injury.
9. What are the long-term implications of untreated plantar fasciitis and Achilles tendonitis?
Untreated plantar fasciitis and Achilles tendonitis can lead to chronic pain, decreased mobility, and functional limitations. In severe cases, persistent inflammation may result in tissue damage and degeneration, requiring more invasive interventions for treatment.
10. When should individuals seek professional help for plantar fasciitis and Achilles tendonitis?
Professional help should be sought if symptoms persist despite conservative measures or if there is a significant impact on daily activities. A healthcare provider specializing in musculoskeletal conditions can conduct a thorough evaluation and recommend appropriate treatment options tailored to individual needs.