Plantar Fasciitis, more than any other problem I encounter is something that many people have just resigned themselves to dealing with. There can be many causes, some of them take a long time to resolve and others take less time. As a general rule, the longer you have been dealing with the condition the longer it will take you to get out of the condition – though there are many notable exceptions to this rule.
The foot and the brain
The feet are the two most important parts of the body when it comes to the single movement that most defines us as human beings: bipedal movement, aka “walking”.
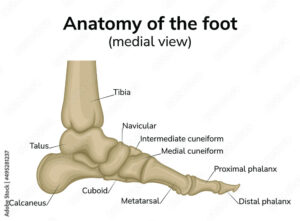
This should come as no surprise to you, because the foot touches the ground…normal walking is impossible without it. Duh. But let me explain some not-so-obvious reasons why the foot, and more specifically the bones & positions of the bones in the foot are so profoundly important to how we move.
Proprioceptors in Ligaments
The talus is one of two bones in the human body that has no muscles attached to it. The talus also supports the entire weight of the body, so you may mistake this bone as merely a piece of structure support. You would be wrong.
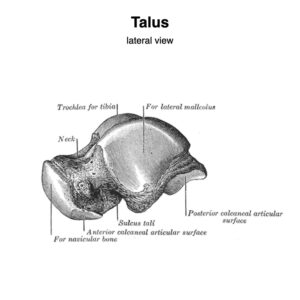
Every ligament in the body is filled with golgi ligament endings – these are special sensory neurons that provide feedback to the brain on the status of a ligament. The talus, with its many ligaments provides important information to the brain about which muscles to activate during gait (aka walking). Improper positioning of the talus will cause erroneus information to be sent to the brain, causing muscles that should support and decelerate the various bones of the foot to misfire. This series of events leads to excess energy being absorbed by the plantar fascia, irritating the fascia and the bone it attaches to – resulting in the all too common “plantar fasciitis”.
The solution – A multimodal approach
To fix plantar fasciitis requires a comprehensive analysis of the positions of the bones of the foot – and a plan to restore their position. In addition strengthening of the misfiring & atrophied muscles is required. Through a combination of manual therapy and a corrective exercise plan we can restore normal foot mechanics and spare the plantar fascia from absorbing excess energy.
If you’re suffering from plantar fasciitis, please contact me

FAQ Section: Plantar Fasciitis Relief in Santa Rosa
1. What causes Plantar Fasciitis and how long does it take to resolve?
Plantar Fasciitis stems from various factors, including improper foot mechanics, overuse, or wearing inadequate footwear. The duration of recovery varies based on individual circumstances. Typically, the longer one has been affected, the more time it may take to fully recover. However, with a tailored treatment plan, significant improvements can be achieved.
2. How does the foot contribute to Plantar Fasciitis?
The foot plays a pivotal role in our biomechanics, particularly in walking or running. The intricate network of ligaments, including those around the talus bone, sends crucial feedback to the brain, guiding muscle activation during movement. Misalignment in the foot, especially the talus, can disrupt this feedback loop, leading to overloading of the plantar fascia and subsequent inflammation.
3. What is the significance of proprioceptors in ligaments concerning Plantar Fasciitis?
Proprioceptors are sensory receptors embedded within ligaments, providing vital feedback on joint position and movement to the brain. In the context of Plantar Fasciitis, the ligaments surrounding the talus bone contain these proprioceptors. Any misalignment in the talus can result in erroneous signals to the brain, causing improper muscle activation and contributing to the condition’s development.
4. How can a multimodal approach aid in relieving Plantar Fasciitis?
A multimodal approach combines various strategies to address Plantar Fasciitis comprehensively. This approach typically involves analyzing foot biomechanics to identify misalignments, followed by manual therapies to restore proper positioning. Additionally, targeted exercises help strengthen weakened muscles and correct imbalances, thereby alleviating strain on the plantar fascia and promoting healing.
5. What role does corrective exercise play in treating Plantar Fasciitis?
Corrective exercises are integral to rehabilitating Plantar Fasciitis. These exercises aim to strengthen weakened muscles, improve flexibility, and correct biomechanical imbalances contributing to the condition. By addressing underlying issues and promoting proper foot mechanics, corrective exercises not only alleviate symptoms but also prevent recurrence.
6. How effective is manual therapy in managing Plantar Fasciitis?
Manual therapy, including techniques such as soft tissue mobilization and joint manipulation, can provide immediate relief from Plantar Fasciitis symptoms. By targeting tight muscles, releasing adhesions, and restoring joint mobility, manual therapy helps reduce pain and inflammation while facilitating the healing process. When combined with other treatment modalities, it enhances overall outcomes for individuals with Plantar Fasciitis.
7. Can custom orthotics help in treating Plantar Fasciitis?
Custom orthotics are often recommended as part of a comprehensive treatment plan for Plantar Fasciitis. These orthotic devices are tailored to individual foot anatomy and biomechanics, providing support and cushioning to alleviate pressure on the plantar fascia. By optimizing foot alignment and distributing weight evenly, custom orthotics help reduce strain on the affected tissues and promote healing.
8. What lifestyle modifications can aid in Plantar Fasciitis recovery?
In addition to targeted therapies, certain lifestyle modifications can support Plantar Fasciitis recovery. These may include wearing supportive footwear with adequate arch support, avoiding activities that exacerbate symptoms, and incorporating stretching and strengthening exercises into daily routines. Maintaining a healthy weight and practicing good foot hygiene also play crucial roles in managing the condition effectively.
9. Are there any preventive measures to avoid Plantar Fasciitis?
While not always preventable, certain measures can reduce the risk of developing Plantar Fasciitis. These include gradually increasing activity levels to avoid overuse injuries, wearing supportive footwear suitable for specific activities, and maintaining a healthy weight to minimize stress on the feet. Regular stretching and strengthening exercises can also help maintain optimal foot mechanics and prevent imbalances that contribute to the condition.
10. When should I seek professional help for Plantar Fasciitis?
If you experience persistent heel pain, especially during weight-bearing activities or upon waking in the morning, it’s advisable to consult a healthcare professional. Early intervention can prevent the worsening of symptoms and expedite recovery. A qualified healthcare provider, such as a podiatrist or physical therapist, can accurately diagnose Plantar Fasciitis and recommend appropriate treatment options tailored to your individual needs.
