“The ultimate mystery is one’s own self.” – Sammy Davis, Jr.
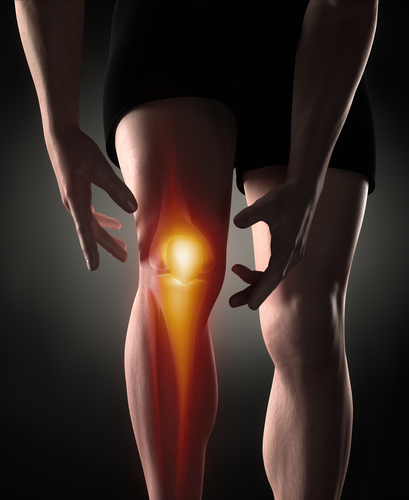
It is a commonly accepted belief in our culture that athletes are more prone than most to joint and muscle injuries and pain. While this may have some basis in fact, the unfortunate truth for most people who do not consider themselves as athletic is that they can suffer many of the same ailments. A common example is a knee pain that can occur on or near the kneecap known as patellofemoral pain syndrome, or PFPS. Patellofemoral pain syndrome is the most common cause of knee pain seen by doctors. And it is one of the most misunderstood.
Understanding Patellofemoral Pain Syndrome
According to the American Academy of Orthopaedic Surgeon’s website:
“Patellofemoral pain syndrome is a broad term used to describe pain in the front of the knee and around the patella, or kneecap. It is sometimes called “runner’s knee” or “jumper’s knee” because it is common in people who participate in sports—particularly females and young adults—but patellofemoral pain syndrome can occur in nonathletes, as well. The pain and stiffness it causes can make it difficult to climb stairs, kneel down, and perform other everyday activities.”
The thing to keep in mind is that anyone can develop patellofemoral pain syndrome, especially if they are physically active or are engage in repetitive actions using their legs and knee joints. There are several factors that may contribute to the onset of PFPS. Overuse from vigorous athletics, training, or repetitive motion are often significant factors as well as issues with the alignment of the kneecap. Your knee is made up of four main components, namely bones, cartilage, ligaments, and tendons. It is also the largest joint in your body as well as one of the most complex. Patellofemoral pain syndrome occurs from pain originating in the soft tissues and bone around the kneecap. These tissues include the tendons, the fat pad beneath the patella, and the synovial tissue that lines the knee joint.
In most cases, PFPS is associated with vigorous physical activities that put repeated stress on the knee —such as running, kneeling or squatting, and climbing stairs. It can also be caused by a sudden change in physical activity such as the frequency of activity or the duration or intensity of activity.
The most common symptom is knee pain that increases with stair climbing or squatting movements. In addition, patients can experience pain after sitting for an extended time with their knees bent, such as watching television or a movie.
Causes and Treatment of Patellofemoral Pain Syndrome
According to the experts at the Mayo Clinic doctors aren’t clear as to the actual causes of patellofemoral pain syndrome, but experience has shown that it is most often associated with:
- Overuse. Running or jumping sports puts repetitive stress on your knee joint, which can cause irritation under the kneecap.
- Muscle imbalances or weaknesses. Patellofemoral pain can occur when the muscles around your hip and knee don’t keep your kneecap properly aligned. Inward movement of the knee during a squat has been found to be associated with patellofemoral pain.
- Injury. Trauma to the kneecap, such as a dislocation or fracture, has been linked to patellofemoral pain syndrome.
- Surgery. Knee surgery, particularly repair to the anterior cruciate ligament using your own patellar tendon as a graft, increases the risk of patellofemoral pain.
Typically, doctors will prescribe rest as a primary treatment. In addition, OTC pain relievers and physical therapy also can also be used to reduce pain.
However, there are other options that can be considered for treatment. One of the issues to bear in mind is that PFPS is a syndrome, not a specific cause. A syndrome is defined as a group of symptoms that consistently occur together or a condition characterized by a set of associated symptoms. Because the cause or causes of these symptoms can be difficult to isolate and identify, treatment options can be a bit generalized.
However, studies have offered consistent evidence that exercise therapy for patellofemoral pain syndrome may result in a measurable reduction in pain and improved functional ability. It can also help to enhance long-term recovery. However, it is still unclear what is the best form of exercise therapy in each case and it is whether these results can be obtained by all people with PFPS. One significant insight from the studies is that hip exercise combined with knee exercises may be more effective in reducing pain than knee exercise alone.
Assessing Your Condition
Initially, we will want to perform a movement and structural assessment using both SFMA and Anatomy in Motion.
The SFMA, or Selective Functional Movement Assessment, is a series of seven full-body movement tests. While these movement tests are relatively simple to do, they provide a foundation for a series of more complex tests that gradually provide us with a path for treatment options.
Anatomy in Motion, or AiM, uses a gait assessment to provide a complete roadmap of the structure of the human body. AiM philosophy is founded on principles of movement that are influenced by our most primal, repetitive, and fundamental movement: walking, or our gait.
By using gait analysis, hands-on assessment, manual therapy, and corrective exercises, Anatomy in Motion can provide a significant improvement in movement mechanics. This, in turn, leads to pain relief, improved functionality, and performance, while improving results from other therapies.
Together, these assessments can give us a more holistic view of your body’s functionality and dysfunctions, if any. Armed with those insights we can develop a therapy approach best suited to treat the underlying causes of your knee pain and the patellofemoral pain syndrome that is hindering you.
Patellofemoral Pain Syndrome and Pain and Performance Solutions
We can help you find the answer to your pain. By setting up your first appointment with us you can begin to start by you telling us what your first injury was. Your first injury is very telling, and we will explain why that is when you come in. Don’t simply ignore your knee pain hoping it will just go away. Let us help. Contact us today at 707-636-4404 or book an appointment online to start your recovery process.
Preventing Patellofemoral Pain Syndrome: Proactive Steps for Long-Term Knee Health
One of the most effective ways to address patellofemoral pain syndrome (PFPS) is through proactive care. For individuals with active lifestyles or jobs that require repetitive knee motions, establishing a knee health routine can help minimize the risk of developing PFPS. Regularly incorporating strengthening and stretching exercises, particularly those targeting the quadriceps, hamstrings, and hips, can improve knee alignment and reduce stress on the patella. Additionally, keeping track of your activity intensity and duration can prevent sudden increases that place extra strain on the knees. Building in rest days and alternating high-impact activities with low-impact ones, like cycling or swimming, is also beneficial for maintaining balanced knee health.
Early Intervention: Recognizing the Signs and Taking Action
Early intervention is key when it comes to managing patellofemoral pain syndrome. Many people may ignore mild knee discomfort, hoping it will resolve on its own. However, addressing symptoms early on can prevent PFPS from progressing to a more painful and persistent condition. Noticing warning signs such as mild soreness around the kneecap, stiffness after sitting for long periods, or discomfort during activities like stair climbing should prompt an assessment with a healthcare provider. By addressing these signs early, you may avoid a long recovery process and reduce the need for more intensive treatments. Consulting a professional for a personalized exercise plan can help manage symptoms and prevent further damage.
Establishing a Knee-Centric Wellness Routine
Creating a knee-centric wellness routine tailored to your lifestyle and activity level can be an excellent way to support long-term knee health. This routine might include warm-up exercises, consistent stretching, and targeted strengthening workouts that engage the surrounding muscles of the knee, hip, and core. Additionally, wearing proper footwear suited to your activities can help maintain alignment and reduce knee stress. Investing in ergonomic aids, such as supportive shoe inserts, can also reduce impact during walking or running. By incorporating these preventive measures and building a consistent wellness routine, you can manage existing PFPS symptoms and significantly reduce the likelihood of future knee pain.